Dr. Perry Nickelston, Core Stability, The Diaphragm & Dysfunctional Breathing
Dr. Perry is world-renown for his contributions within the musculoskeletal world. Check out stopchasingpain.com and his podcasts.
Here, he discusses mobility vs stability. You can be as mobile as you want, but if you lack the stability to get you there, you’re going to get hurt. Your core helps control and regulate intrinsic abdominal pressure – the pressure required to help you brace for any physical activity. Can’t squat worth a damn, but you’re big and strong – fix your breathing first and watch the weight go up.
Taping the Diaphragm
By Perry Nickelston, DC, FMS, SFMA
The human body possesses the power of reacting to gravity, inertia and momentum, the primary forces of the physical world, by means of proprioception: “perceiving self.” This proprioceptive system helps guide total-body reaction to the outside world and gives us awareness of space and time. It is a critical player in organization, function, timing and sequencing when moving!
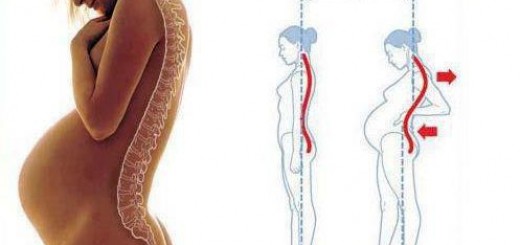
Muscle sequencing and timing are fundamental in the movement game. If you want to get from Point A to Point B, you need proximal stability for optimal distal mobility. Stability determines performance. You can have all the mobility you need for movement, but without stability you cannot control power and strength. Proprioception is the linchpin between stability and mobility.
If the central core cylinder of your body is unstable, the nervous system inherently restricts mobility to obtain the necessary stabilization. It locks down joints (fixation) in a primal attempt at stabilization for self-preservation. Dysfunctional breathing patterns often occur after an injury as a stress protective mechanism.
Altered breathing is often a contributing factor to injury because of its impact on functional intra-abdominal pressure (IAP). It may also negatively impact proprioceptive feedback of the core. Elastic therapeutic taping techniques can be an effective proprioceptive feedback tool for your patients, helping reset the “feel” of optimal breathing patterns.
How can tape impact proprioception? Proprioceptive response via stimulation to the skin is significantly faster than visual or auditory input. This is critical in restoring reactive, fundamental movement patterning and sequencing. The “touch” or “feel” of tape via the sensory motor skin mechanoreceptors heightens neural communication with the brain, helping restore postural control and muscle memory. Tape consciously and unconsciously stimulates movement patterning.
The Intrinsic Core
What exactly is the core? For the purpose of this article we will be discussing the inner-unit “intrinsic” core subsystem. The intrinsic core is comprised of the transverse abdominis, lumbar multifidi, diaphragm and pelvic floor. One may also include the deep neck flexors and posterior fibers of the internal obliques because they relate to the deep fascial core referenced in Thomas Myers’ Anatomy Trains.
These inner-unit structures form a postural stabilization support cylinder via intra-abdominal pressure; think Valsalva maneuver. Due to the stresses of life, movement dysfunction, past injuries, trauma, and pain compensations, the inner-core unit often becomes compromised.
Past pain syndromes and injuries often lead to lumbar multifidi, transverse abdominis, and pelvic floor inhibition with diaphragm facilitation. In simple terms, some muscles do too much; others don’t do enough. (Side note: Some therapy techniques refer to a dysfunctional diaphragm as being inhibited; not working efficiently. The terms facilitated or inhibited may be interchangeable depending on your therapeutic background. The important takeaway point is: The diaphragm does not work efficiently).
Dysfunctional Breathing
 Dysfunctional breathers use too much chest and scalene recruitment instead of the diaphragm, adding stress to the vulnerable anterior kinetic chain. Functional breathing via abdominal and full rib-cage expansion is difficult for many patients to accomplish. Their brain has simply forgotten how to “do it” and “feel it.” Your goal is to help them remember and teach them how to do it on their own. Properly applied tape to the diaphragm will give them the necessary critical feedback to learn this pattern. Remember, respiration is a subconscious action. It happens automatically so we don’t perish. Breathing is a conscious action. We can control howit’s done.
Dysfunctional breathers use too much chest and scalene recruitment instead of the diaphragm, adding stress to the vulnerable anterior kinetic chain. Functional breathing via abdominal and full rib-cage expansion is difficult for many patients to accomplish. Their brain has simply forgotten how to “do it” and “feel it.” Your goal is to help them remember and teach them how to do it on their own. Properly applied tape to the diaphragm will give them the necessary critical feedback to learn this pattern. Remember, respiration is a subconscious action. It happens automatically so we don’t perish. Breathing is a conscious action. We can control howit’s done.
There is a “functional” and a “dysfunctional” way to breathe. Sadly, the majority of people have faulty breathing patterns that may contribute to movement impairments and chronic musculoskeletal pain syndromes. Since the diaphragm itself does not hurt, it is often overlooked a causative factor in pain.
Breathing plays a pivotal role in posture, limb function, spine mobility, and lumbopelvic hip stabilization via intra-abdominal pressure mechanisms. Diaphragm fascial attachments to the spine, psoas, quadratus lumborum, thoracolumbar fascia, internal organs and pelvic floor make it the keystone of dynamic core stabilization.
Taping the Diaphragm to Help Normalize Breathing
So, how does one go about normalizing breathing patterns? Proper breathing involves the diaphragm contracting to compress the abdominal cavity, making more space for the lungs to expand. The best way to assess this: With the patient in a seated position, palpate the lower ribs, the sides of the abdomen and the iliac crest, and have them breathe. Ideally, the patient will expand ribs into your hand with minimal elevation of the rib cage until late in the breathing cycle.
Envision inflating a balloon that expands 360 degrees. It’s not simply expanding the abdomen, but involving the entire rib cage. This is known as “360-degree breathing.” This is often the most difficult part of the movement for patients to feel. If they are unable to breathe efficiently in a seated position, regress them to an unloaded supine position requiring less core stabilization.
According to fitness professional Carson Boddicker: “Normal breathers should take between 10,000 and 14,000 breaths per day; however, ‘over breathers’ do a lot more, slightly smaller ‘reps.’ Retraining of a good diaphragmatic breathing pattern can begin to normalize the amount of CO2 (carbon dioxide) within the system by slowing down breathing and resetting the brain’s perception of ‘normal’ blood gas levels.”
Manual release of the facilitated diaphragm based on your own therapeutic techniques should precede taping. The patient should be taped in the standing position (see taping tips below and accompanying video). Once taped, have the patient lie down in the supine position, knees bent and feet flat, to begin practicing diaphragmatic breathing.
Proprioceptive feedback from the tape on the transverse abdominis, rectus abdominis, obliques, rib cage, and thoracolumbar fascia will be very helpful for your patient in “feeling” the ideal sequencing. Having the 24/7 support of the tape once they leave your office will help prevent reverting back to faulty breathing patterns. Tape can remain on for 3-5 days, and another application can then be applied if indicated.
Taping Technique Tips
- Patient should stand with hands over head to stretch the rib-cage depressors.
- Start tape just below sternum. Follow the rib-cage line posterior.
- Do not stretch the tape. Simply follow the rib-cage line.
- Cross midline posterior and tape down toward the opposite hip.
- Posterior tape should cross at the proximal attachment of the quadratus lumborum and intersection of thoracolumbar fascia.
Adding taping techniques to your program of restorative breathing and therapeutic core strengthening exercises may help accelerate recovery. Patients love the feel of the tape and will typically ask for more. Increasing stability is the name of the movement game. Breathing and taping can be your go-to game changers.
Resources
- Boddicker C. “Diaphragmatic Breathing: What Are We Changing?” Aug. 6, 2010.
- Cook G. Movement: Functional Movement Systems : Screening, Assessment, and Corrective Strategies. Aptos, CA: On Target Publications, 2010.
- “Performance Diaphragm Power Taping” (video). Rocktape.com.
- Todd ME. The Thinking Body. New York: Dance Horizons, 1975.
- Weinstock D. NeuroKinetic Therapy: An Innovative Approach to Manual Muscle Testing. Berkeley, CA: North Atlantic, 2010.
Original Article by: Dr. Perry Nickelston at Dynamic Chiropractic