
Fascia is a web of fibrous tissue that permeates the body, but is it really the “Cinderella Tissue”that new age therapists, Rolfers, and yoga instructors suggest? The fascial system is still a medical mystery. But that could soon change, thanks to an unlikely alliance between researchers and alternative therapists.
Image of myofacial release therapy via Colorado Body and Soul
In October, 2007, more than 100 scientists from around the world convened in Boston, Massachusetts to discuss the latest research on fascia, an enigmatic, gauze-like matrix of connective tissue that envelopes the muscles, surrounds the nerves and swathes the organs in a body-wide-web of fibrous collagen. But the researchers had some unlikely company. Also in attendance, and outnumbering researchers 5:1, was a throng of complementary- and alternative-medicine practitioners with a mutual interest in fascia. United by their fascination with this medically neglected tissue, the two camps comprised the attendees of the first-ever International Fascia Research Congress.
Science‘s coverage of that first congress indicates that practitioners of complementary and alternative medicine (aka “CAM”) signed up for the meeting in droves. The researchers, however, had required some convincing. Therapies defined by the National Institutes of Health as “complementary,” “alternative,” or “integrative,” are characterized, in large part, by a lack of scientific evidence in support of their effectiveness. More distasteful, still, to many scientists, is how readily such therapies expose themselves to untestable spiritual and metaphysical interpretations. For many researchers, to associate with alternative practitioners is to not only grant outlandish theories credibility by association, but to risk sullying one’s own scientific reputation.
The scientists who did attend the meeting had been assembled through the efforts of conference-founder and Executive Director Thomas Findley. An MD with a PhD in physical medicine and rehabilitation, Findley has studied the science of rehabilitation for close to forty years. But he is also a longtime practitioner of “Rolfing.” Also known as “Structural Integration,” Rolfing is an alternative form of movement and energy therapy. To quote Ida P. Rolf, the founder of the practice:
Rolfers make a life study of relating bodies and their fields to the earth and its gravity field, and we so organize the body that the gravity field can reinforce the body’s energy field. This is our primary concept.
But unlike many alternative therapists, Findley seems to recoil at the mention of words like “energy field.” Among bodyworkers like Rolfers, the standard practice may be to offer therapies that elude quantification and verification, but this, Findley says, is problematic. “The point of science is to ask a question in a way that can be answered either ‘yes’ or ‘no,'” he says, “and a lot of practitioners pose questions in ways that aren’t really answerable in a scientific context.” [At left: The logo for the Rolf Institute of Structural Integration, which markets Rolfing. According to the RISI, Rolfing “works on the web-like network of connective tissues, called fascia, to release,realign and balance the whole body, potentially resolving discomfort, reducing compensations and alleviating pain.”]
Findley thinks the answers he’s looking for could be hiding in fascia. On the scientific side of things, the field of fascia research has grown considerably in recent years, though it lacks the coherence of other, more established areas of physiological investigation. For decades, anatomical dissections and representations have presented the body as stripped of its fascial tissues, and the majority of physiology textbooks make little mention of it. “Most scientists,” says Wallace Sampson, alternative medicine skeptic and professor emeritus at Stanford University, “even those wary of alternative therapies, admit that the field of fascia research is a field of neglect, and remains sorely under-investigated.”
By uniting alternative therapists with researchers, Findley hopes to spur discovery. He is fond of telling conferencegoers that when he was in medical school, glial cells (the predominant cell-type in the central nervous system) had no function. “We now know [glial cells] have a major function in memory, and do all sorts of things,” he says. “What about fascia?”
“We strip it, do away with it, say it has no function at all,” he continues. “Well, I suspect we’re going to find major functions in fascia, just as we find major functions in glial cells.”
Growing Acceptance
It’s been almost seven years since the first Fascia Research Congress, and both Findley and his conference have celebrated their fair share of accomplishments. World-renowned biomechanics researcher Peter Huijing, who was reluctant to attend the first FRC for fear that it would damage his reputation, has become one of the biggest headliners at subsequent meetings. He volunteered to help organize the second FRC in 2009. He even convinced his home institution – Vrije Universiteit Amsterdam – to host it.
In 2007, Wallace Sampson, the alternative medicine skeptic, roundly criticized the Fascia Research Congress, calling it “A Meeting of Incompatibles.” You have to do the basic science and build from there, he insisted at the time. “You can’t force the clinical side.” In 2014, Sampson applauds Findley. “Findley may be in a position to point out, better than anyone else, in any other field, the reasons for the conflict between alternative medicine and basic science,” he told me.
And yet, fascia’s “major functions” have yet to reveal themselves. To date, there have been no home runs establishing a clear, causal link between fascia’s molecular, cellular, or biomechanical properties and the effective treatment of pain, injury, or disease – at least to the satisfaction of the broader scientific community. Findley continues to reference discoveries that have yet to be made. His e-mail signature is a quote, attributed to Albert Einstein.
“For an idea that does not first seem insane,” it reads, “there is no hope.”
But how insane is Findley’s idea, really? Does it not make intuitive sense that a tissue found throughout the body would harbor some form of medical or therapeutic significance?
Sure, says John Hutchinson, professor of evolutionary biomechanics at University of London’s Royal Veterinary College, but intuition can be dangerous when it comes to research. “There’s a lot about it we don’t understand,” he says, noting that it remains an understudied tissue, “but when you point to something as complex as fascia, it’s easy to use the fact that it’s understudied in a way that’s convenient to your argument.”
Robert Schleip – a longtime Rolfer turned researcher, and director of Ulm University’s Fascia Research Group – has expressed similar frustrations over what he calls “the current trend among bodyworkers of attributing anything wonderful or astonishing to the properties of fascia”:
[Our research group] has been receiving an almost exponentially increasing number of inquiries from enthusiastic healers (and martial art teachers) worldwide who wish that we would sanctify their claims that fascial contraction provides the explanation for their observed miracle powers. While I do tend to believe that the fascial net plays much larger roles in human functioning than previously assumed in orthopedic medicine, I am afraid that such over-zealous claims and projections are undermining the seriousness of the investigation.
In a presentation delivered at the 2012 International Fascia Research Congress (a video of which appears below), Schleip expanded on this point in a talk about how his experience as a scientist has informed his personal Rolfing practice:
“We have been teaching for several decades that with the rolfing strokes we are changing a gel-to-sol transition int he ground substance, or that we are also loosening cross-links within the collagen fibers,” says Schleip, in reference to common phrases employed by Rolfers to explain their work to their patients. “But, if you meet us teachers late night at the bar, we don’t know shit about it and we agree to that.”
To quote Eric Jacobson – a lecturer on Global Health and Social Medicine at Harvard Medical School with longstanding ties to the Rolf Institute of Structural Integration, the Ida P. Rolf Research Foundation, and the Fascia Research Congress – the current state of fascia science is such that one must always bear in mind “the difference between what we know about fascia and what we’re hypothesizing its significance might be.”
What Does Medical Science Know About Fascia?
Scientific investigations of fascia have grown considerably in recent years, as evidenced by a continuous rise in its MEDLINE references since the 1960s. Suffice to say, there is more research to summarize than there is space to do so. Science writer Paul Ingraham sums up a great deal of this work in his article “Does Fascia Matter?”
Robert Schleip sent me six scientific articles that he regards as “home runs” for the field of clinical fascia research (see references below). I showed the studies to Hutchinson and to Silvia Blemker, a biomedical engineer at the University of Virginia.
Blemker says the the clinical studies Schleip references “all provide evidence to support the role of fascia in health and disease, but… they are small bits and pieces of the puzzle and in many ways do not fit within the community’s conceptual models of disease processes.” In this light, she continues, “it is understandable that these studies get push-back from the [larger scientific community.]”
Neither of the rodent studies seemed particularly momentous to Hutchinson. “Even considered together and taken rather credulously in terms of the details of the science, these two rat studies seem incremental to me.” As part of a sustained research effort, Hutchinson says it’s possible these studies might eventually dovetail with others and lead to some improvements in care. “Possibly,” he hedges, “or not.”
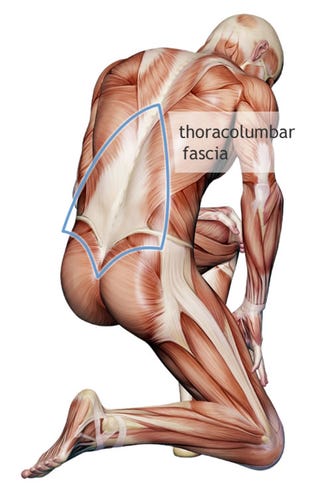
Hutchinson’s language echoes that of Rolfing-researcher Eric Jacobson, who had the following to say at a recent presentation on the therapeutic implications of the lumbar fascia – a collagenous sheet that spans and connects to various bones and regions of the back:
The hypothesis now is that maybe chronic low back pain has something to do with a dysfunction in that fascia. [That] it’s at least part of the story, maybe.
Both Hutchinson and Blemker had good things to say about Huijing’s work, but they agree that it raises more questions than it answers.
Scientists know, for example, that fascia surrounds, separates and connects muscles throughout the body. According to Blemker, Huijing and his colleagues have developed a long line of research demonstrating fascia’s ubiquity in the body enables it to transmit some degree of force within and between muscles, but “this line of thinking has yet to adopted by the mainstream biomechanics community because it does not yet fit within our conceptual model of musculoskeletal function.”
“There’s no question Huijing’s work is fascinating,” adds Hutchinson, “and there are aspects about myofascial force transmission that may be right. We just don’t know how right, and how generalizable it would be, yet.”
At least in the eyes of Hutchinson and Blemker, these are not “home runs.” Are they interesting? Yes. Deserving of further investigation? Absolutely. But the therapeutic benefits of fascial manipulation remain too poorly understood to inform therapeutic interventions.
“Once you say something is not well known,” Hutchinson says, “then as far as science is concerned, as far as evidence-based medicine is concerned, that’s where you stop. You don’t elevate it to some other level of significance.”
Ingraham, for his part, draws a similar conclusion:
Fascia is biologically interesting! All biology is. But clinical relevance is the central question of this article: if fascia science cannot actually improve treatment, then it makes no sense to be fascinated by it in a therapeutic context.
The New Age Tradition vs. Science
Where do new age ideas about fascia originate? To hear Findley tell it, therapies exist that have targeted fascia for thousands of years. But his personal views on fascia, and the ethos of the Fascia Research Congress as a whole, have been informed in large part by the writings ofAndrew Taylor Still, the 19th Century founder of osteopathic medicine. Writes Findley, in an essay titled “The Fascia Research Congress from the 100 year perspective of Andrew Taylor Still”:
I was fortunate in 1988 to inherit the library of more than 100 journal articles… which included the writings on fascia by AT Still. I knew there was important information there, but did not examine them closely until an Osteopathic student was doing a research rotation with me in 2012. The first three fascia congresses thus evolved from 2007 to 2012 without the benefit of guidance from Dr Still, but remarkably cover most of the concepts he proposed in his writings.
The essay reveals how much Findley’s work is influenced by Still’s osteopathic philosophy, which he summarizes in four points:
1. The human body functions as a total biologic unit
2. The body possesses self-healing and self-regulatory mechanisms
3. Structure and function are interrelated, and
4. Abnormal pressure in one part of the body produces abnormal pressures and strains upon other parts of the body.
Sampson says Findley’s references to Still (pictured above, photo via LOC), and other anatomical concepts that developed in the 1800s, reflect an anachronistic approach to science.
“Still and his contemporaries had concepts that they described in terms of wholeness, proper function, and the like,” says Sampson. These are words that accommodate innumerable little reactions, associations and constructions of the human body, and of life in general. The problem, says Sampson, is that when we talk about “wholeness,” “proper function,” “total function,” “intact function” and so forth, we do so with words “whose definitions we understand, but whose underlying meanings we do not.”
The Future of Fascia Research
Sampson comments on the limitations of language are especially timely, in light of an ongoing debate within the field of fascia research. A recent issue of the Journal of Bodywork and Movement devoted no fewer than six editorials to the lack of agreement over what should or should not be referred to as “fascia.” To hear contributor Paolo Tozzi tell it, “there is no area of anatomical science stigmatized by a larger divergent terminology as the one regarding fascia-related connective tissue.”
The issue of nomenclature was first brought to the table in an editorial by University of Padova anatomist Carla Stecco, first author of one of the “home run” studies sent to me by Schleip. She summarizes the problem with fascia nomenclature as follows:
Fascia is often described as an ubiquitous tissue that permeates the human body, organized as a three-dimensional network that surrounds, supports, suspends, protects, connects and divides muscular, skeletal and visceral components of the body. If we agree with this wide definition [Ed. Note: There are definitions still more expansive than this one. See this popular definition, which classifies even cartilage and bone as fascia.], then fasciae could include every connective tissue, loose or dense, regular and irregular, with so many functions that would be impossible to study and understand from a scientific point of view.
Responses from Stecco’s fellow contributors on the matter range from supportive:
“…inconsistent usage of anatomical terms makes it difficult to compare results across research studies and to draw generalized conclusions. This is a serious problem that will slow progress if not addressed. “
- University of Vermont neuroendocrinologist Helene Langevin (another researcher cited by Schleip)
To, at times, borderline dismissive:
In the absence of another word, ‘fascia’ has a popular meaning that is in such widespread use that we should ‘go with it’ for our communication with the world of the public and large groups of practitioners.
-Tom Myers, author of Anatomy Trains, a popular guide to myofascial therapy for manual and movement therapists
The most telling editorial of all, however, may be the one penned by Leon Chaitow, the journal’s Editor in Chief, titled “Can We Describe What We Do?”, in which he notes:
It seems… that detail of a single manual method might need to incorporate a dozen or more descriptors. And since, in many manual treatment settings a range of methods are involved in a single session – precise replication, based on such descriptions, would at times be extremely difficult, if not impossible, to realise.
The upshot? No. Bodyworkers, including those who purport to target fascia in a therapeutic fashion, cannot describe what they do. At least not currently. ” This might not be an impossible task, but it would certainly require focused attention from many for a considerable time,” concludes Chaitow (who, it bears mentioning, sits on the Board of Directors of the Ida P. Rolf Research Foundation, as well as its Science Advisory Council). “Are we prepared for such a task?”
Sampson says Chaitow, Schleip, Findley, and anyone else who straddles the divide between researcher and alternative practioner must be, if they are to elevate the field of therapeutic fascial manipulation to a new plane of biomedical legitimacy.
“I applaud them,” says Sampson, noting that he took away more from the First International Fascia Research Congress than he had anticipated. “I spent considerable time reviewing the research that was presented, and learned a lot from it.” But demonstrating the therapeutic benefits of fascial manipulation, which he concedes is “an interesting concept,” cannot be accomplished through language and thought alone. It has to be through mathematics, and statistics, observation, repeated observation and validation. It must be based in reproducibility, “not feedback into your fingers.”
Sampson says that attempting to unite traditional and alternative medicines – an undertaking he initially condemned – has put Findley in a unique position to explore the divide in alternative medicine. “Dr. Findley strikes me as a reasonable, sensible person” he says “one who could keep the organization on track,” even as “attempts to find connections to function and therapy fail.” Such an endeavor, he says “could lead one to see the futility of extending connections too far beyond reasonable probability.”
“Tell doctor Findley and his crew that ‘it’s tough,'” Sampson says. “And i don’t mean ‘tough titties.’ I mean to say that it is very hard.”
“That’s life,” he says. “That’s science. We do the best we can.”
References
Papers that Robert Schleip recommends on fascia:
- Huijing – “Epimuscular myofascial force transmission: a historical review and implications for new research”
- Tesarz et al. – “Sensory innervation of the thoracolumbar fascia in rats and humans. Neuroscience.”
- Langevin et al. – “Reduced thoracolumbar fascia shear strain in human chronic low back pain”
- Schilder et al. – “Sensory findings after stimulation of the thoracolumbar fascia with hypertnoic saline suggest its contribution to low back pain”
- Corey et al. – “Stretching of the back improves gait, mechanical sensitivity and connective tissue inflammation in a rodent model”
- Stecco et al. – “Ultrasonography in myofascial neck pain: randomized clinical trial for diagnosis and follow-up”
Original Article by: Robbie Gonzalez at io9.com





